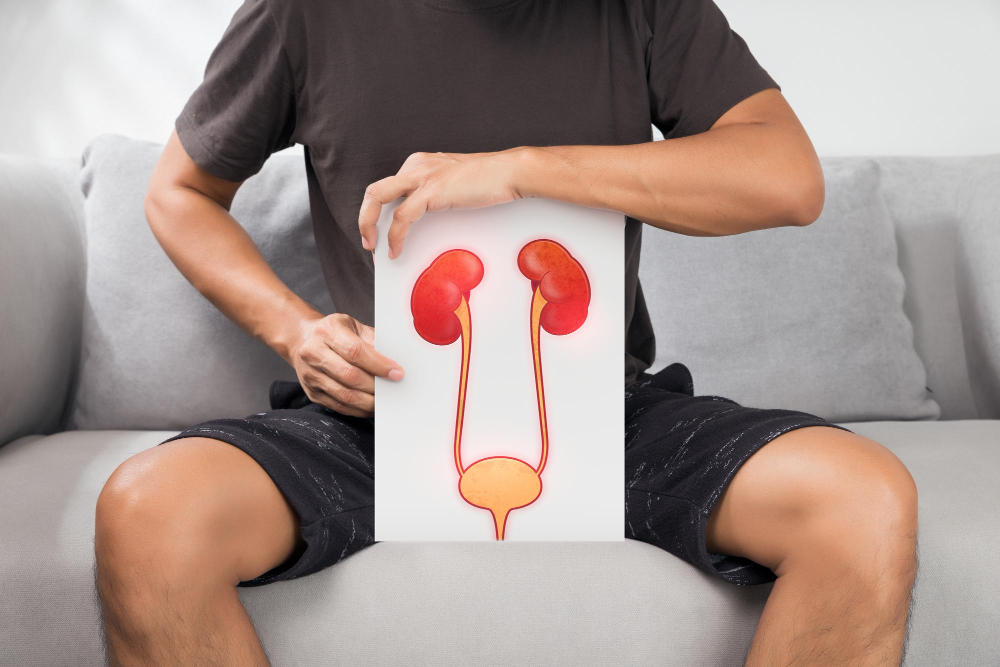
The bladder, located in the lower abdomen, is a crucial organ that stores urine until it is ready to be expelled from the body. Normally, the process of urination is regulated by a complex interaction of muscles and nerves that work together to store and release urine at the appropriate time. Signals travel from the brain through the spinal cord to the muscles in the bladder and urinary sphincter, coordinating their actions to control urination.
In a healthy bladder, nerves send signals to the brain when it’s time to urinate, prompting the bladder muscles to contract and the sphincter to relax, allowing urine to flow out. However, when nerve pathways are disrupted due to injury, disease, or other conditions, this communication system breaks down, leading to a condition known as neurogenic bladder. In neurogenic bladder, the nerves responsible for controlling bladder function are impaired, which can result in either an overactive bladder (frequent urges and inability to fully retain urine) or an underactive bladder (difficulty emptying the bladder).
Neurogenic bladder is associated with numerous neurological conditions, including stroke, spinal cord injuries, Parkinson’s disease, multiple sclerosis, and diabetic neuropathy. The National Institute of Neurological Disorders and Stroke (NINDS) provides detailed information on how neurological conditions affect the nervous system, including conditions that can lead to neurogenic bladder.
Causes of Neurogenic Bladder
Several neurological conditions and injuries can disrupt bladder nerve function, leading to neurogenic bladder. Some of the most common causes include:
1. Spinal Cord Injuries (SCI)
Injuries to the spinal cord are a major cause of neurogenic bladder. SCI can interrupt the signals sent between the brain and the bladder muscles, resulting in loss of bladder control. Depending on the level and severity of the injury, the bladder may either become overactive (spastic bladder) or underactive (flaccid bladder).
- Spastic Bladder: This condition, often resulting from injuries above the sacral spinal cord, causes involuntary bladder contractions, leading to frequent urges and potential incontinence.
- Flaccid Bladder: When the injury is lower or involves the sacral spinal cord, it may cause an underactive bladder, leading to difficulties in starting urination and fully emptying the bladder.
For more on spinal cord injuries and their effects on bladder function, refer to the National Institute of Neurological Disorders and Stroke (NINDS).
2. Stroke and Stroke Recovery
A stroke, caused by the interruption of blood flow to the brain, can damage areas that control bladder function. Individuals recovering from stroke may develop neurogenic bladder, either as an overactive or underactive bladder. Patients with stroke-induced neurogenic bladder may require bladder training and physical therapy to regain control over urination.
3. Multiple Sclerosis (MS)
Multiple sclerosis, a condition where the immune system attacks the protective covering of nerve fibers, disrupts nerve signals between the brain and the rest of the body. MS frequently affects bladder function, resulting in urinary urgency, frequent urination, or difficulty emptying the bladder. For more information on MS and its effects, visit the National Multiple Sclerosis Society.
4. Parkinson’s Disease
Parkinson’s disease, a progressive neurological disorder, affects muscle control and coordination. Many individuals with Parkinson’s experience bladder issues, particularly an overactive bladder due to increased muscle activity. Symptoms may include a frequent need to urinate, urgency, and even incontinence.
5. Diabetic Neuropathy
Diabetes, particularly when poorly managed, can lead to nerve damage over time. This condition, known as diabetic neuropathy, often affects the bladder nerves, causing neurogenic bladder. Individuals with diabetic neuropathy may have an underactive bladder, resulting in difficulty starting urination and incomplete bladder emptying.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) provides resources on diabetic complications, including neurogenic bladder.
6. Trauma and Surgery
Pelvic trauma or surgeries that affect the nerves in the pelvic area can result in neurogenic bladder. For example, prostate surgery in men or hysterectomy in women can sometimes damage the nerves controlling bladder function, leading to symptoms of neurogenic bladder.
7. Other Neurological Conditions
Conditions such as spinal tumors, encephalitis, herniated discs, and even certain autoimmune diseases can impair bladder control. Any condition that affects the brain, spinal cord, or nerves linked to bladder function has the potential to cause neurogenic bladder.
Symptoms of Neurogenic Bladder
Symptoms of neurogenic bladder depend on whether the bladder is overactive (spastic) or underactive (flaccid). Common symptoms include:
Overactive Bladder (Spastic)
- Frequent Urination: Individuals may feel the need to urinate frequently, even with small amounts of urine.
- Urgency: There is a sudden, uncontrollable urge to urinate, which may lead to incontinence if a restroom is not readily available.
- Nocturia: Frequent urination at night, which disrupts sleep.
Underactive Bladder (Flaccid)
- Difficulty Starting Urination: Many people experience trouble initiating the flow of urine, which can be both uncomfortable and frustrating.
- Inability to Fully Empty the Bladder: This symptom leads to a feeling of fullness and discomfort in the lower abdomen, increasing the risk of urinary tract infections (UTIs).
- Overflow Incontinence: Due to the bladder overfilling, urine may leak involuntarily.
- Inability to Sense Bladder Fullness: Individuals may not feel the urge to urinate, leading to accidental leakage.
For more information on symptoms and coping with bladder control issues, refer to resources from the Centers for Disease Control and Prevention (CDC).
Diagnosing Neurogenic Bladder
Accurate diagnosis of neurogenic bladder is essential to tailor the most effective treatment plan. Physicians rely on a combination of physical examinations, patient history, and specialized tests to diagnose the condition.
- Medical History and Physical Examination: A thorough history of the patient’s health and any previous neurological conditions or injuries is critical. A physical examination can help identify contributing factors, such as diabetes or Parkinson’s disease.
- Urodynamic Studies: Urodynamic testing evaluates how well the bladder, sphincter, and urethra store and release urine. It can help determine whether the bladder is overactive, underactive, or obstructed.
- Post-Void Residual (PVR) Measurement: This test measures the amount of urine left in the bladder after urination using ultrasound or a catheter. High PVR indicates incomplete bladder emptying, common in underactive neurogenic bladder.
- Imaging Tests: Ultrasound, MRI, or CT scans provide visual assessments of the bladder, kidneys, and surrounding structures, identifying any structural abnormalities.
- Cystoscopy: A cystoscope, a thin tube with a camera, is inserted into the urethra to inspect the bladder for abnormalities.
- Neurological Exams: Since neurogenic bladder is linked to neurological conditions, physicians often perform additional neurological tests to assess brain and nerve function.
Treatment Options for Neurogenic Bladder
Treatment options for neurogenic bladder focus on improving quality of life, managing symptoms, and preventing complications such as infections or kidney damage. Approaches vary depending on the underlying cause, bladder function, and severity of symptoms.
1. Behavioral and Lifestyle Modifications
- Bladder Training: Bladder training involves scheduled voiding to encourage regular urination, which can help improve bladder control over time. This technique is particularly helpful for overactive bladder.
- Fluid Management: Adjusting fluid intake to avoid excessive hydration before bed can help reduce nighttime urination. Avoiding caffeine, alcohol, and acidic beverages may also improve bladder control.
2. Pelvic Floor Exercises
Pelvic floor exercises, or Kegel exercises, strengthen the muscles that support the bladder and urinary sphincter. Strengthening these muscles can improve bladder control and reduce leakage. Kegel exercises can benefit both overactive and underactive bladder cases. For guidance on performing pelvic floor exercises, refer to the National Institute on Aging (NIA).
3. Medications
Several medications are available to manage neurogenic bladder symptoms:
- Anticholinergics: Drugs such as oxybutynin and tolterodine help relax the bladder muscle, reducing urgency and frequency for those with overactive bladder.
- Botulinum Toxin (Botox): Botox injections into the bladder muscle can reduce overactivity by temporarily paralyzing the muscle, which may help reduce urinary urgency and frequency.
- Alpha-Blockers: For patients with difficulty voiding, alpha-blockers like tamsulosin can relax the bladder neck muscles, making urination easier.
- Cholinergic Agents: For underactive bladder, cholinergic drugs such as bethanechol stimulate bladder contractions, aiding in complete voiding.
4. Intermittent Catheterization
Intermittent self-catheterization is recommended for individuals with underactive bladder who cannot empty the bladder completely. This involves using a catheter to drain urine at regular intervals. While it can initially be challenging, many patients find that self-catheterization provides relief from symptoms and reduces the risk of infections.
5. Electrical Stimulation Therapy
Electrical stimulation, particularly sacral neuromodulation (SNS), uses mild electrical impulses to stimulate nerves that control bladder function. An implantable device delivers these impulses, helping to normalize bladder contractions and reduce urgency, frequency, and incontinence. SNS can be an effective option for patients with refractory symptoms who have not responded to other treatments. The U.S. Food and Drug Administration (FDA) provides additional information on the safety and usage of neuromodulation devices.
6. Surgical Options
Surgery is typically a last resort for individuals with neurogenic bladder who have not responded to other treatments.
- Urinary Diversion: In severe cases where bladder function cannot be restored, urinary diversion surgery reroutes urine flow. This surgery may involve creating a stoma (opening) on the abdomen for urine collection.
- Augmentation Cystoplasty: This procedure involves enlarging the bladder with a patch made from intestinal tissue, allowing the bladder to hold more urine.
Managing Life with Neurogenic Bladder
Living with neurogenic bladder can be challenging, but lifestyle adjustments, support, and medical intervention can improve the quality of life. Here are some tips:
- Follow a Routine: Regular bathroom visits and fluid management can help avoid overfilling the bladder and reduce urinary urgency.
- Infection Prevention: Since incomplete bladder emptying can lead to UTIs, maintaining cleanliness and drinking adequate water can help prevent infections.
- Support and Education: Support groups, either online or in-person, can be invaluable for sharing experiences and coping strategies. Educating oneself about neurogenic bladder can empower individuals to manage their symptoms effectively.
Conclusion
Neurogenic bladder is a complex condition requiring a multidisciplinary approach to treatment. With proper diagnosis and a tailored treatment plan, many people with neurogenic bladder can regain control over their bladder function, reduce symptoms, and lead fulfilling lives. For additional information, the National Institutes of Health (NIH) offers resources on neurogenic bladder, related conditions, and current research.