Minimally invasive urologic surgery encompasses a range of surgical techniques designed to treat various conditions within the urinary tract and male reproductive organs with reduced impact on the body. Unlike traditional open surgery, which requires large incisions, minimally invasive surgery (MIS) uses small incisions, specialized instruments, and advanced technology, allowing surgeons to perform precise and effective procedures with minimal damage to surrounding tissues.
In recent years, minimally invasive approaches have become the preferred choice for many urologic surgeries, including treatments for kidney stones, prostate issues, and bladder conditions. With these procedures, patients experience less pain, reduced scarring, and faster recovery times. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), minimally invasive options offer effective solutions for a wide array of urologic conditions, ensuring patients receive innovative and compassionate care.
Common Types of Minimally Invasive Urologic Surgeries
Minimally invasive urologic surgeries encompass a wide range of procedures, each tailored to treat specific conditions. Here are some of the most common types:
1. Laparoscopic Surgery
Laparoscopic surgery is a form of MIS that involves small incisions through which a camera and specialized instruments are inserted to perform the procedure. The surgeon views the area on a monitor, allowing precise movements with minimal disruption to surrounding tissues.
- Common Uses: Laparoscopic surgery is used for kidney removal (nephrectomy), adrenal gland removal, ureteral repair, and treatment of kidney stones.
- Benefits: Less blood loss, reduced risk of infection, and quicker recovery time compared to traditional open surgery.
2. Robotic-Assisted Surgery
Robotic-assisted surgery utilizes a robotic system, typically the da Vinci Surgical System, to enhance precision and flexibility. The surgeon controls robotic arms equipped with tiny instruments, allowing fine movements that may be challenging with human hands alone. Robotic-assisted surgery is especially useful for delicate or complex urologic surgeries.
- Common Uses: This approach is frequently used for prostate removal (prostatectomy), kidney surgery, and reconstructive urologic procedures.
- Benefits: Greater precision, reduced trauma to surrounding tissues, and often better preservation of nerve function, which can be critical in procedures like prostatectomy.
3. Endoscopic Surgery
Endoscopic surgery, also known as cystoscopic or ureteroscopic surgery, involves inserting a thin, flexible tube with a camera (endoscope) through the natural openings of the body, such as the urethra, to reach the urinary tract. This approach requires no external incisions and allows for a detailed view of the urinary tract.
- Common Uses: This method is commonly used for treating bladder tumors, kidney stones, and ureteral strictures.
- Benefits: No external incisions, minimal recovery time, and reduced risk of infection.
4. Percutaneous Nephrolithotomy (PCNL)
Percutaneous nephrolithotomy is a minimally invasive procedure to remove large or complex kidney stones that cannot be treated with less invasive methods. A small incision is made in the back, allowing direct access to the kidney to remove the stone.
- Common Uses: PCNL is typically used for larger kidney stones or when other methods, like lithotripsy, are ineffective.
- Benefits: Direct removal of stones with fewer complications compared to open surgery.
5. Laser Surgery
Laser surgery uses high-energy laser beams to break up kidney stones, remove tumors, or treat benign prostatic hyperplasia (BPH). The laser can precisely target tissue, minimizing damage to surrounding areas.
- Common Uses: Laser surgery is used for treating BPH (laser prostatectomy) and breaking down kidney stones (laser lithotripsy).
- Benefits: Precise treatment, minimal bleeding, and faster recovery times.
For more information on types of urologic surgeries, refer to resources provided by the National Institutes of Health (NIH).
Benefits of Minimally Invasive Urologic Surgery
Minimally invasive techniques offer a range of benefits over traditional open surgery, improving patient outcomes and enhancing the overall surgical experience. Some of the key advantages include:
- Smaller Incisions and Reduced Scarring: Minimally invasive surgeries use smaller incisions than traditional open surgeries, leading to less visible scarring and faster wound healing.
- Less Pain and Discomfort: With less tissue disruption and smaller incisions, patients typically experience less post-operative pain, reducing the need for pain medication and enhancing comfort during recovery.
- Shorter Hospital Stays: Many minimally invasive procedures can be performed on an outpatient basis, allowing patients to return home the same day or with a shorter hospital stay compared to open surgery.
- Faster Recovery Times: Patients undergoing MIS often resume normal activities sooner, thanks to reduced trauma to the body and faster healing.
- Lower Risk of Infection and Complications: Smaller incisions and shorter hospital stays contribute to a lower risk of surgical site infections and other complications.
- Greater Precision and Accuracy: Techniques like robotic-assisted surgery enable higher precision, minimizing damage to surrounding nerves and tissues, which can be crucial in surgeries like prostatectomy.
For further reading on the benefits of minimally invasive surgery, visit the Centers for Disease Control and Prevention (CDC).
Risks and Considerations
While minimally invasive urologic surgery offers many benefits, it’s important to understand potential risks and limitations:
- Surgical Complications: As with any surgery, risks include bleeding, infection, and adverse reactions to anesthesia.
- Conversion to Open Surgery: In some cases, complications during a minimally invasive procedure may require a conversion to open surgery for patient safety.
- Learning Curve: Certain techniques, such as robotic-assisted surgery, require specialized training. Choosing a surgeon experienced in MIS is essential for minimizing risks and achieving the best outcome.
For patients considering surgery, discussing potential risks and benefits with a healthcare provider can help determine the best approach.
Preparing for Minimally Invasive Urologic Surgery
Preparation for minimally invasive surgery is similar to other types of surgery, although each procedure may have specific requirements. Here are some general steps to prepare:
- Pre-Operative Assessment: Patients typically undergo a thorough evaluation, including blood tests, imaging studies, and possibly an electrocardiogram (EKG) to assess their overall health.
- Medication Adjustments: Certain medications, such as blood thinners, may need to be temporarily stopped to reduce bleeding risks. It’s important to inform the healthcare provider about all medications, including supplements.
- Fasting Requirements: Patients are often instructed not to eat or drink for a specific period before surgery to ensure safety during anesthesia.
- Pre-Surgery Instructions: Surgeons may provide specific instructions, such as bowel preparation or antiseptic bathing, to reduce infection risks.
For more information on preparing for surgery, consult the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
The Procedure: What to Expect During Minimally Invasive Urologic Surgery
Minimally invasive urologic surgery is usually performed under general or regional anesthesia. While each procedure varies, here’s a general overview of what to expect:
- Anesthesia: Depending on the procedure, general anesthesia or regional anesthesia (such as spinal or epidural) may be used to ensure patient comfort.
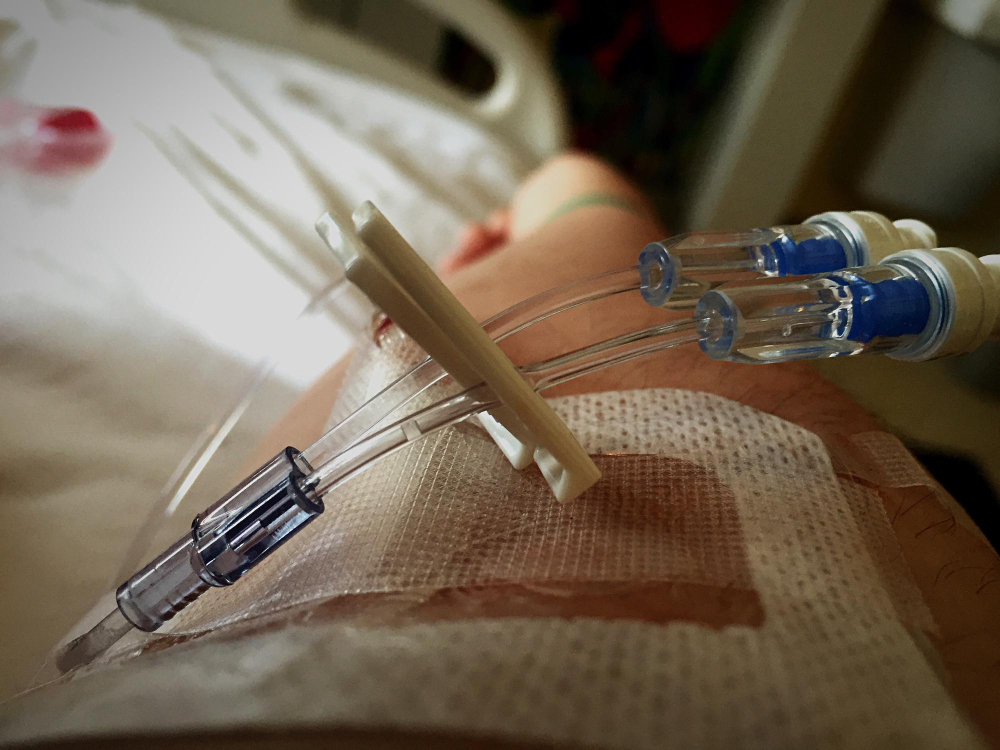
- Incisions and Access Points: The surgeon makes small incisions through which instruments, cameras, and other devices are inserted. In robotic-assisted surgery, robotic arms hold and maneuver these instruments.
- Monitoring and Precision: With real-time imaging on a monitor, the surgeon performs the procedure, using advanced tools to treat the targeted area with precision.
- Completion and Closure: Once the procedure is complete, the surgeon removes the instruments and closes the incisions with stitches or surgical glue.
After surgery, patients are moved to a recovery area to be monitored as the anesthesia wears off. Many patients are discharged on the same day or after a brief hospital stay.
Recovery After Minimally Invasive Urologic Surgery
Recovery times for minimally invasive surgeries are generally shorter than for open surgeries, but the exact duration varies depending on the procedure and individual health. Here are some tips and expectations for recovery:
- Managing Pain and Discomfort: While pain is usually mild, over-the-counter pain relievers or prescribed medications can help manage discomfort. Patients should follow the surgeon’s guidance on medication use.
- Resuming Activity: Light activities can typically be resumed within a few days, but strenuous activities, including heavy lifting and vigorous exercise, should be avoided until the healthcare provider approves.
- Caring for Incisions: Incision sites should be kept clean and dry. Patients are usually advised to avoid soaking in water (like in baths or pools) until the incisions have fully healed.
- Follow-Up Appointments: Follow-up visits allow healthcare providers to monitor healing, assess for complications, and ensure that the procedure successfully addressed the condition.
- Signs of Complications: Patients should watch for signs of infection (redness, swelling, or discharge at the incision site), fever, or unusual pain, and contact their healthcare provider if these symptoms occur.
For additional recovery tips, refer to the American Urological Association (AUA).
Conditions Commonly Treated with Minimally Invasive Urologic Surgery
Minimally invasive techniques are commonly used to treat a range of urologic conditions, including:
- Benign Prostatic Hyperplasia (BPH): Minimally invasive treatments, such as transurethral resection of the prostate (TURP) and laser therapy, help alleviate urinary symptoms caused by an enlarged prostate.
- Kidney Stones: Procedures like laser lithotripsy and percutaneous nephrolithotomy (PCNL) are effective for removing kidney stones.
- Prostate Cancer: Robotic-assisted prostatectomy offers a precise method for removing the prostate with minimal impact on surrounding tissues.
- Bladder Cancer: Endoscopic surgeries enable the removal of small tumors from the bladder lining with minimal trauma.
The National Cancer Institute (NCI) provides additional resources on cancer treatment options, including minimally invasive surgery.
Living with a Urologic Condition Treated with Minimally Invasive Surgery
Living with a urologic condition can be challenging, but minimally invasive surgery provides an effective treatment option that reduces recovery time and helps individuals return to daily activities more quickly. Patients are encouraged to maintain open communication with their healthcare providers, adhere to follow-up care instructions, and monitor any symptoms that may arise post-surgery.
Conclusion
Minimally invasive urologic surgery has transformed the field of urology, offering effective treatments with less impact on the body, reduced recovery times, and fewer complications. For those facing urologic conditions requiring surgical intervention, minimally invasive techniques provide a modern, patient-centered approach to treatment. Discussing options with a urologist and understanding what to expect can help ease concerns and lead to a successful outcome.
For more information on minimally invasive urologic surgery and related treatments, visit the National Institutes of Health (NIH).